Spondylolisthesis – Isthmic
Spondylolisthesis – Isthmic
Spondylolisthesis is a condition of spinal instability, in which one vertebra slips forward over the vertebra below. Isthmic spondylolisthesis, the most common form of this condition, is caused by a bony defect (or fracture) in an area of the pars interarticularis, an area located in the roof (laminae) of the vertebral structure.
This bony defect occurs in approximately 4% of the population, and results from a genetic failure of bone formation. The condition most commonly affects the fourth and fifth lumbar vertebrae (L4 and L5) and the first sacral vertebra (S1). It is interesting to note that the condition is not always painful.
Symptoms
Symptoms of isthmic spondylolisthesis may include the following:
- Pain in the low back, thighs, and/or legs – especially after exercise – that radiates into the buttocks
- Muscle spasms
- Leg pain or weakness
- Tight hamstring muscles
- Irregular gait
Some people are symptom free and only discover the disorder when seeing a doctor for another health problem. In severe cases, the condition may cause swayback and a protruding abdomen, a shortened torso, and a waddling gait.
What Causes Isthmic Spondylolisthesis?
Isthmic spondylolisthesis can be the result of a genetic failure of bone formation in the spinal vertebrae. Usually physical stresses to the spine then break down the weak or insufficiently formed vertebral components. Repeated heavy lifting, stooping, or twisting can cause small fractures to occur in the vertebral structure and lead to the slippage of one vertebra over another. Weightlifters, football players, and gymnasts often suffer from this disorder due to the considerable stress placed on their spines.
Diagnosis
To make an accurate diagnosis, Dr. Lonner will conduct a careful and rigorous diagnostic process, including:
- Medical history. The physician will talk to you about your symptoms, how severe they are, and what treatments you have already tried.
- Physical examination. You will be carefully examined for limitations of movement, problems with balance, and pain. During this exam, the doctor will also look for loss of reflexes in the extremities, muscle weakness, loss of sensation or other signs of neurological damage.
- Diagnostic tests. Generally, doctors start with plain x-rays, which allow us to rule out other problems such as tumors and infections. We may also use a CT scan or MRI to confirm the diagnosis. In some patients we may need a myelogram. This is a test that involves the use of a liquid dye that is injected into the spinal column to show the degree of nerve compression and slippage between involved vertebrae.
Grading a Spondylolisthesis
There are several methods used to “grade” the degree of slippage ranging from mild to most severe. Your surgeon will discuss with you the extent of your spondylolisthesis and how the severity indicates the type of treatment that is needed.
In general, most physicians use the Meyerding Grading System for classifying slips. This is a relatively easy to understand system. Slips are graded on the basis of the percentage that one vertebral body has slipped forward over the vertebral body below. Thus a Grade I slip indicates that 1-24% of the vertebral body has slipped forward over the body below. Grade II indicates a 25-49% slip. Grade III indicates a 50-74% slip and Grade IV indicates a 75%-99% slip. If the body completely slips off the body below it is classified as a Grade V slip, known as spondyloptosis.
Dr. Lonner will consider the degree of slip, and such factors as intractable pain and neurological symptoms, when deciding on the most suitable treatment. As a general guideline, the more severe slips (especially Grades III and above) are most likely to require surgical intervention.
Non-Operative Treatment
For most cases of isthmic spondylolisthesis (especially Grades I and II), treatment consists of temporary bed rest, restriction of the activities that caused the onset of symptoms, pain/ anti-inflammatory medications, steroid-anesthetic injections, physical therapy and/or spinal bracing.
Surgical Treatment
Surgery is rarely needed unless the case is severe (usually Grade III or above), neurological damage has occurred, the pain is disabling, or all non-operative treatment options have failed.
The most common surgical procedure used to treat spondylolisthesis is called a laminectomy and fusion. In this procedure, the spinal canal is widened by removing or trimming the laminae (roof) of the vertebrae. This is done to create more space for the nerves and relieve pressure on the spinal cord. The surgeon may also need to remove all or part of the vertebral disc (discectomy) and then also fuse vertebrae together. If fusion is done, various devices (like screws or interbody cages) may be implanted to enhance fusion and to support the unstable spine.
Case Examples of Isthmic Spondylolisthesis
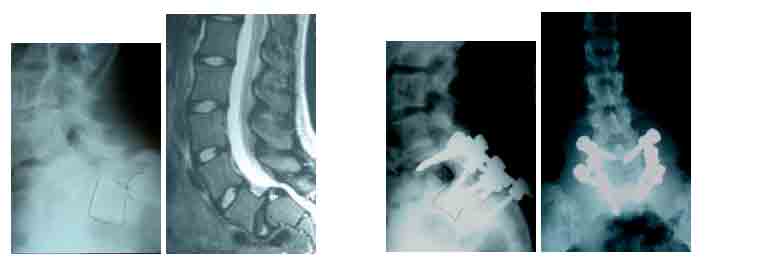
This adolescent girl had a high-grade spondylolisthesis of L5/S1. The pre-operative x-ray and MRI reveal the severity of the slip before surgery. The slip was corrected from a posterior approach with fusion and instrumentation. The patient is over 4 years out from surgery and is active and without back pain.
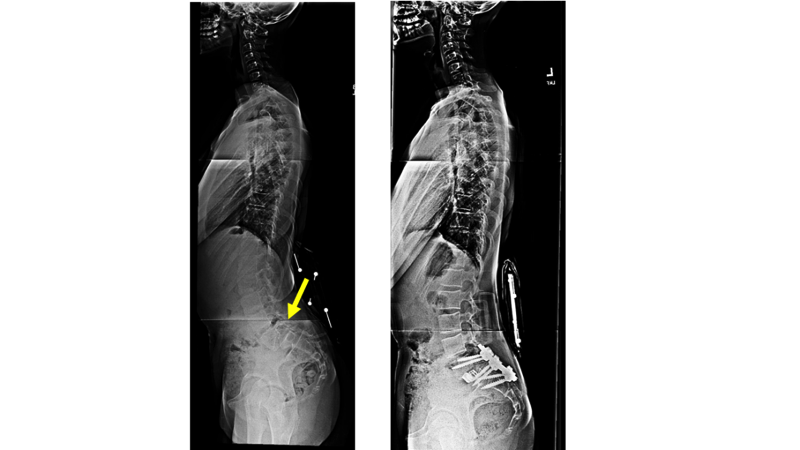
This 16 years old girl had a severe isthmic spondylolisthesis (slip) with severe back pain, leg pain, and difficulty standing upright. Dr. Lonner performed a procedure called a reduction in which the slipped vertebra is brought back into its proper position and a fusion is performed. This young lady was able to return to full activity 3 months after surgery.
While it may not be possible to prevent all spine problems, there are things you can do to help keep your spine healthy. The most important prevention method is to avoid or limit those work or recreational activities that cause considerable stress to your spine. Losing weight, starting a regular exercise regimen, not smoking, and learning proper body mechanics can all help reduce the risk of further back problems.